Introduction
Acute transfusion reactions (ATRs) have a broad spectrum of presentations ranging from benign to life-threatening. Due to the rarity of these reactions, there is a paucity of data regarding their incidence and clinical outcomes. The objectives of this study were to determine the incidence of ATRs, its risk factors, and associated mortality.
Methods:
We reviewed the National Inpatient Sample (NIS) database 2014 for admissions where the patient (>=18 years old) was transfused blood products. The NIS is a large publicly available all-payer inpatient healthcare database designed to produce U.S. regional and national estimates of inpatient utilization, access, charges, quality, and outcomes. ATRs were identified using ICD-9 CM codes for transfusion-associated circulatory overload (TACO), transfusion-related acute lung injury (TRALI), febrile non-hemolytic transfusion reactions (FNHTR), acute infections, anaphylaxis, and acute hemolytic reaction. Pearson's chi-square and student's t-test were used to compare categorical and continuous variables between hospitalizations with versus without ATRs, respectively. Multivariate logistic regression analysis was done to determine the risk factors for common ATRs (TACO, TRALI, and FNHTR). A multivariate cox proportional model was built to compare the mortality of two study groups. A 2-sided p-value ≤ 0.05 was considered significant.
Results:
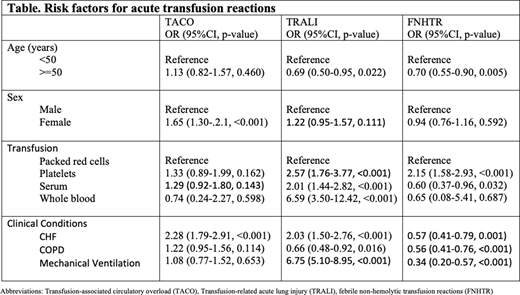
A total of 2,134,691 hospitalizations were associated with the transfusion of blood products. ATRs were documented in 0.2% of the hospitalizations (TACO 0.08%, TRALI 0.06%, FNHTR 0.09%, others 0.003%). The group that had ATRs was slightly younger (median age 67 vs 68 years, p=0.002), had the same proportion of females (58.3% vs 55.3%, p=0.055), less comorbidity score (28.7% vs 31.7% had Charlson Comorbidity Index >3, p=0.042) and more critically ill (17.8% vs 10.5% on mechanical ventilation, p<0.001) compared to group without ATRs. Hospitalizations with ATRs had longer median length of stay (7 vs 6 days, p<0.001) and higher median hospital cost ($64,399 vs $53,912, p<0.001) compared to without ATRs. The risk factors for common ATRs (odds ratio, OR) are mentioned in the table. ATRs were not associated with increased risk of mortality (combined HR 0.89 95%CI 0.71-1.12, p=0.321).
Conclusions:
Nationally, the incidence of ATRs is low in hospitalized patients and it is not associated with increased mortality. This large database analysis gives insight into the risk factors associated with different ATRs.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal